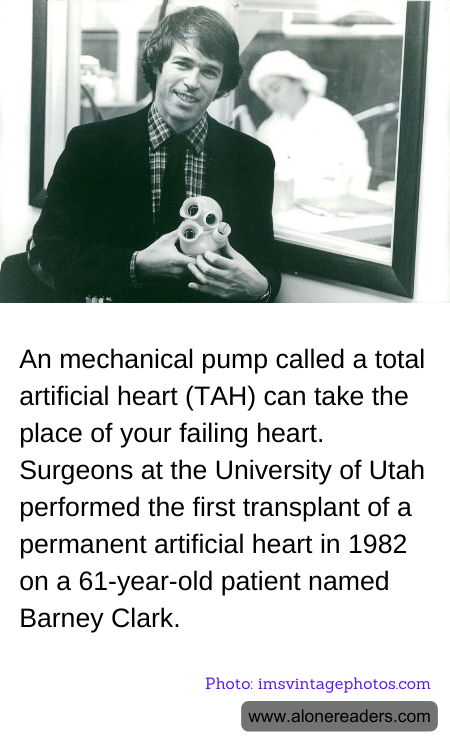
The total artificial heart (TAH) represents a significant advancement in medical technology, primarily aimed at providing a bridge to transplants or, at times, a permanent solution for patients suffering from end-stage heart failure. In an extraordinary leap in medical science, surgeons at the University of Utah made history in 1982 by successfully implanting the first permanent artificial heart in a 61-year-old dentist named Barney Clark. This groundbreaking procedure marked a pivotal moment in the evolution of biomedical engineering and its application in medicine.
Barney Clark survived for 112 days post-operation with the artificial heart, a device called the Jarvik-7, named after its designer Dr. Robert Jarvik. The Jarvik-7 was a pneumatic system, driven by a compressor outside the body. This device was not without its challenges, including infections, strokes, and other complications, highlighting the complexities and risks associated with such high-stakes medical interventions. However, it also opened the door to the possibility of replacing diseased hearts without the need for a human donor heart, which are in limited supply.
Following the case of Barney Clark, total artificial hearts have significantly evolved with advances in materials, design, and technology. Modern artificial hearts are more compact, reliable, and capable of being used not just as temporary measures but, in some cases, as long-term solutions to heart disease. These devices are generally used in two scenarios: as a bridge to heart transplantation, giving the patient more time until a suitable donor heart is found, or as a destination therapy for those who are not candidates for a transplant.
Despite the innovative progress and the successful deployment of TAHs, there are ongoing challenges such as the risk of blood clots, device malfunction, and the body's reaction to foreign materials. Nevertheless, continuous improvements in sensor technology, materials, and energy sources aim to mitigate these risks and enhance the functionality and integration of artificial hearts within the body.
In conclusion, the development and refinement of the total artificial invasion heart represent a beacon of hope for many facing life-threatening heart diseases, expanding the horizon of therapeutic options beyond the limits of biological organ transplantation. As technology progresses, the integration of these mechanical pumps continues to redefine the landscape of cardiac care, offering promises of extended life, improved quality of life, and new frontiers in medical treatment and research.