Varicose veins are a common yet often misunderstood complication during pregnancy. These bulging, twisted veins typically appear on the legs, but can also develop in the vulva and rectum (hemorrhoids). Although usually harmless, they can cause discomfort, pain, and long-term vascular issues if left unmanaged. Understanding their causes and applying targeted preventive strategies is essential for maintaining maternal vascular health.
The physiology of varicose veins
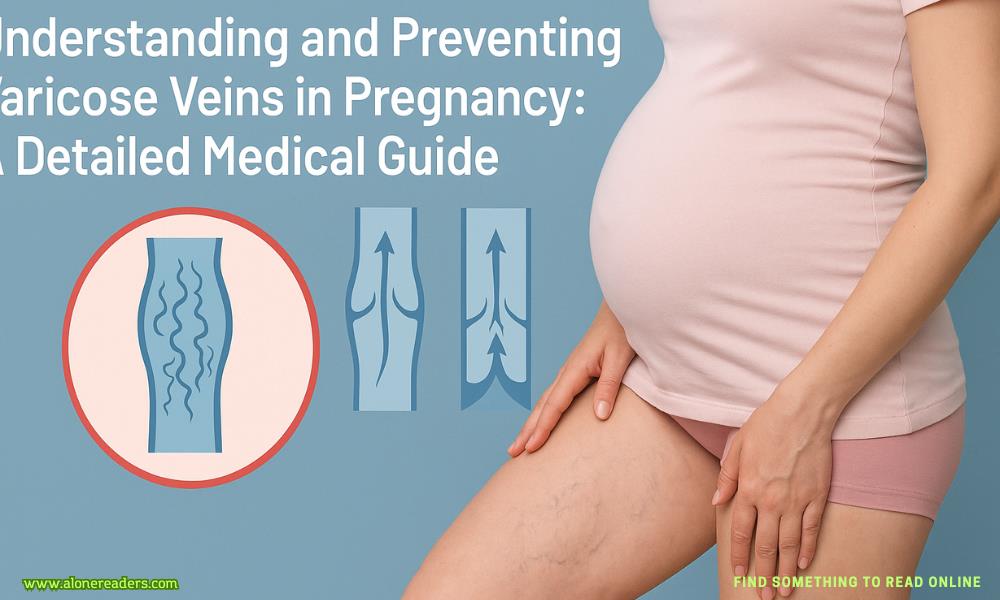
Varicose veins are dilated superficial veins that result from weakening or damage to the vein walls and valves. Normally, valves in the veins prevent backflow of blood, ensuring one-way flow toward the heart. During pregnancy, increased blood volume and hormonal changes lead to venous dilation and valve incompetence, which causes blood to pool in the lower extremities.
Hormonal impact
Progesterone levels rise during pregnancy, relaxing smooth muscle in the blood vessels. This makes the veins more elastic, but also more prone to stretching and weakening. The vascular walls lose tone, and the valves may not close efficiently, promoting reflux.
Mechanical pressure
As the uterus enlarges, it compresses the inferior vena cava and pelvic veins, reducing venous return from the legs. This mechanical obstruction, particularly noticeable in the third trimester, significantly increases venous pressure in the lower limbs.
Genetic predisposition
Women with a family history of venous insufficiency are more likely to develop varicose veins. Pregnancy amplifies this inherited vulnerability due to the compounded effects of hormonal and mechanical changes.
Visible signs
Physical symptoms
Vulvar and pelvic varicosities
In some pregnancies, varicose veins can appear in the vulvar area, leading to localized swelling, pressure, and discomfort during walking or intercourse. These are more common in multiple pregnancies or when standing for long periods.
Thrombophlebitis
Inflammation of varicose veins can cause superficial thrombophlebitis, presenting as a painful, red, and hardened vein. Though superficial, it may require medical attention.
Venous ulceration (rare)
Long-standing venous hypertension can impair skin nutrition, leading to dermatitis or ulcers, though this is rare in pregnancy due to its temporary nature.
Deep vein thrombosis (DVT)
Although varicose veins alone don’t cause DVT, pregnancy already increases the risk of blood clots. If varicosities are extensive, particularly in the pelvic region, and symptoms like unilateral swelling, redness, or pain develop, further evaluation is necessary.
Psychological impact
Visible varicose veins can affect a pregnant woman’s body image and confidence, especially when they are severe. Addressing concerns empathetically is crucial during prenatal care.
1. Compression therapy
Medical-grade compression stockings are the most effective non-invasive intervention. Graduated compression (e.g., 20–30 mmHg) promotes upward blood flow and reduces pooling. They should be worn first thing in the morning before swelling starts.
2. Optimal leg positioning
Encourage frequent elevation of the legs above heart level (e.g., lying on a sofa with legs propped on cushions). Avoid prolonged sitting or standing without movement. Small foot movements or calf contractions every 20–30 minutes help prevent stagnation.
3. Regular physical activity
Low-impact exercises improve venous return. Recommended options include:
4. Sleeping position
Sleep on the left side to reduce pressure on the inferior vena cava and improve venous drainage from the lower body. Use a pillow between the legs to align the pelvis and support vascular flow.
5. Weight management
Excess weight adds strain to the venous system. Gaining only the recommended amount of weight (based on BMI) during pregnancy helps reduce unnecessary pressure on leg veins.
6. Clothing choices
Avoid tight clothing around the waist, groin, or thighs, which can restrict venous outflow. Opt for loose, breathable maternity wear and supportive undergarments designed for pregnancy.
7. Hydration and fiber intake
Straining during bowel movements can exacerbate varicosities, especially in the rectum. High fluid intake and a diet rich in fiber prevent constipation, lowering intra-abdominal pressure.
8. Avoiding high heels
High-heeled shoes reduce calf muscle effectiveness, impairing venous return. Flat or low-heeled shoes that support the arch and allow normal gait are preferred.
While mild varicose veins are normal in pregnancy, certain symptoms necessitate medical evaluation:
Doppler ultrasound may be used to assess blood flow and exclude thrombosis if needed.
In many cases, pregnancy-related varicose veins improve within 3 to 4 months postpartum as hormonal levels normalize and abdominal pressure decreases. However, some may persist or worsen with each subsequent pregnancy.
For persistent or severe varicosities, postpartum treatments may include:
Consultation with a vascular specialist postpartum can guide treatment timing, especially if family planning is ongoing.
Varicose veins during pregnancy are more than a cosmetic concern—they reflect significant physiological changes in vascular dynamics. By understanding their root causes and implementing targeted prevention strategies, pregnant women can mitigate discomfort and reduce long-term risks. Early intervention, medical-grade compression, and consistent lifestyle adjustments play a vital role in managing vein health effectively throughout pregnancy and beyond.