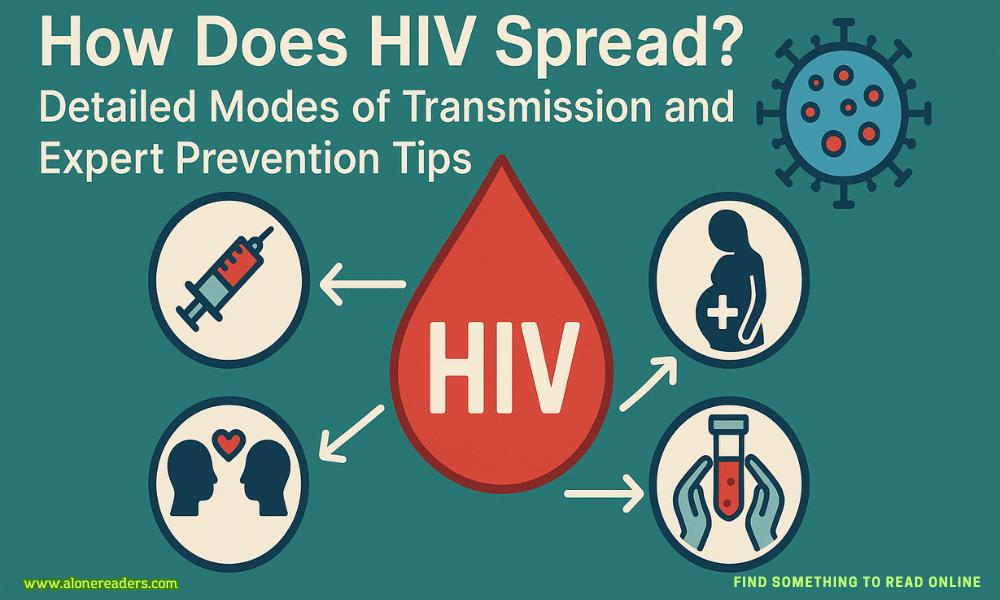
Human Immunodeficiency Virus (HIV) is one of the most extensively studied viruses in the world, yet misconceptions about how it spreads continue to fuel stigma and increase risk. Understanding HIV transmission in detail is crucial for both personal safety and public health. In this comprehensive article, we will explore the exact mechanisms through which HIV is transmitted, clarify common myths, and provide actionable prevention strategies based on current scientific evidence and specialist insights.
Definition and Impact
HIV is a retrovirus that primarily attacks the body’s immune system, specifically targeting CD4+ T lymphocytes, a type of white blood cell essential for immune defense. Over time, untreated HIV weakens the immune system, leading to Acquired Immunodeficiency Syndrome (AIDS), making the body vulnerable to opportunistic infections and certain cancers.
Key Point:
Transmission requires the presence of the virus in sufficient quantities and access to the bloodstream or mucous membranes.
Sexual contact is the most common route for HIV transmission globally. However, not all sexual acts carry the same risk.
Unprotected Vaginal Sex
Unprotected Anal Sex
Oral Sex
Factors That Increase Sexual Transmission Risk
HIV spreads efficiently through direct blood-to-blood contact.
Sharing Needles and Syringes
Blood Transfusions and Organ Transplants
Accidental Needle Sticks (Healthcare Settings)
Healthcare workers face some risk through accidental injuries with sharp instruments (needlesticks), though prompt post-exposure management (PEP) greatly reduces risk.
HIV can be passed from an HIV-positive mother to her child:
During Pregnancy
Virus can cross the placental barrier, especially if the mother has a high viral load.
During Childbirth
Exposure to maternal blood and genital secretions puts the baby at risk.
Through Breastfeeding
Prevention Measures:
Occupational Exposure (Non-Healthcare)
Rare, but possible in certain environments like waste management or laboratories if protocols aren’t followed.
Tattooing, Piercing, and Cosmetic Procedures
Risk exists if equipment is not properly sterilized between uses.
Blood Rituals or Traditional Practices
Any ritual involving the exchange of blood (e.g., scarification, blood brotherhood) carries risk if instruments are shared.
Casual Contact
Shaking hands, hugging, sharing utensils, or using public toilets pose zero risk.
Saliva, Tears, Sweat
These fluids do not contain enough virus to transmit HIV.
Mosquitoes and Insect Bites
HIV cannot survive or replicate in insects. Transmission via mosquito or bug bites is not possible.
Coughing, Sneezing, Airborne Droplets
HIV is not spread through the air.
Viral Load
Presence of STIs
STIs can cause sores or inflammation, facilitating easier entry of HIV.
Type of Exposure
Deep tissue or mucous membrane exposure increases risk compared to superficial contact.
Preventive Interventions
Timely use of post-exposure prophylaxis (PEP) can prevent infection if started within 72 hours after potential exposure.
Use Condoms Correctly and Consistently
Latex or polyurethane condoms reduce the risk of HIV and other STIs when used for every act of vaginal, anal, or oral sex.
Consider PrEP (Pre-Exposure Prophylaxis)
Regular STI Screening and Treatment
Get tested for HIV and other STIs regularly if you are sexually active, especially with new or multiple partners.
Open Communication with Partners
Discuss HIV status and prevention methods with all sexual partners.
Limit Number of Sexual Partners
Reducing the number of partners can lower risk.
Never Share Needles or Injection Equipment
Check the Safety of Blood Products and Medical Procedures
Ensure all blood transfusions, organ transplants, and medical/dental procedures use screened blood and sterilized equipment.
Safe Practices in Tattoo and Piercing Studios
Confirm that all equipment is single-use or properly sterilized.
Access Antenatal Care and HIV Testing
All pregnant women should be tested for HIV as early as possible.
Adherence to Antiretroviral Therapy
HIV-positive mothers must take prescribed medications throughout pregnancy and breastfeeding to minimize transmission risk.
Special Delivery and Feeding Guidelines
Follow healthcare provider recommendations regarding delivery method and infant feeding.
Seek Medical Attention Immediately
Testing and Follow-up
Early testing is essential for accurate diagnosis and prompt treatment if needed.
Adherence to ART
Regular use of antiretroviral medications keeps viral load low and prevents transmission.
Regular Health Monitoring
Ongoing medical follow-up ensures optimal health and reduces risk to partners.
Safe Sex and Disclosure
Using condoms and disclosing status to sexual partners supports mutual safety and informed decision-making.
HIV transmission occurs through specific, well-understood routes—unprotected sex, direct blood exposure, and from mother to child. Understanding the exact ways HIV spreads, and how it does not, is essential for breaking stigma and protecting yourself and others. Prevention strategies are highly effective when implemented correctly, from condom use and PrEP to safe injection practices and maternal care. The fight against HIV is grounded in knowledge, responsibility, and compassion, making education the most powerful tool in ending the epidemic.