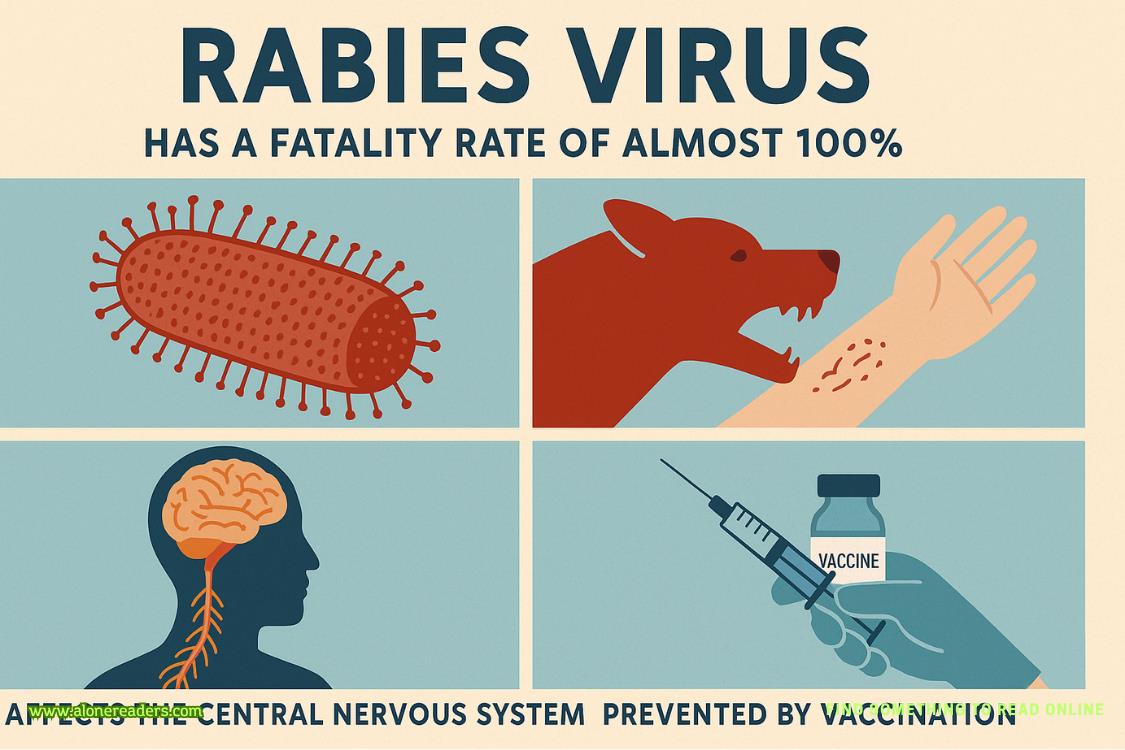
Rabies is one of the deadliest viral diseases known to humankind, notorious for its almost 100% fatality rate once clinical symptoms appear. The disease is caused by the rabies virus, a highly neurotropic virus that specifically targets the central nervous system. This virus is classified as a zoonotic pathogen, meaning it can be transmitted from animals to humans, and it poses a significant threat to both public health and animal populations worldwide.
The rabies virus belongs to the Lyssavirus genus in the family Rhabdoviridae. It is a bullet-shaped virus that is primarily transmitted through the saliva of infected mammals, most commonly through bites. While dogs are the principal reservoir and transmitter in many regions, particularly in Asia and Africa, rabies can also be spread by bats, raccoons, skunks, foxes, and other wild animals. In countries where canine rabies has been controlled or eliminated, wildlife species become the main source of human infections.
When the rabies virus enters the body, usually through a bite wound, it begins its deadly journey toward the brain. Initially, the virus replicates in muscle tissue at the site of entry. It can remain undetected by the immune system for days to months, depending on the location and severity of the wound, the amount of virus inoculated, and the proximity of the bite to the brain. After this incubation period, the virus binds to nicotinic acetylcholine receptors at the neuromuscular junction and starts traveling along the peripheral nerves toward the central nervous system via retrograde axonal transport.
The moment the virus reaches the spinal cord and brain, the symptoms of rabies begin to manifest. Early symptoms can be non-specific and include fever, headache, and general malaise. As the infection progresses, patients develop neurological symptoms such as agitation, confusion, anxiety, and difficulty swallowing. One of the hallmark signs of rabies is hydrophobia, or fear of water, which occurs due to painful throat spasms when attempting to swallow liquids. Hallucinations, hyperactivity, and seizures may occur as the brain becomes increasingly affected. Eventually, the infection leads to paralysis, coma, and, almost inevitably, death within days after the onset of symptoms.
The near-universal fatality rate of rabies after symptom onset underscores the virus’s fearsome reputation. Very rarely, a handful of survivors have been documented, most of whom underwent aggressive, experimental treatment protocols, but such cases are the exception rather than the rule. The reason for the virus’s lethality lies in its ability to evade the immune system during the early stages and its relentless destruction of neural tissue once in the central nervous system.
Despite the grim prognosis of clinical rabies, the disease is entirely preventable through timely intervention. Rabies prevention is based on three pillars: responsible animal vaccination, public health education, and post-exposure prophylaxis for humans. Vaccination of domestic animals, especially dogs, has been the single most effective strategy in reducing the incidence of rabies worldwide. Mass dog vaccination campaigns have led to dramatic declines in human rabies deaths in several countries. In areas where wildlife are major reservoirs, oral vaccination of wild animal populations has also been employed with considerable success.
For humans, prevention hinges on two key strategies: pre-exposure vaccination for high-risk individuals and immediate action following potential exposure. People at increased risk, such as veterinarians, animal handlers, laboratory workers, and travelers to endemic areas, are often advised to receive the rabies vaccine as a preventive measure. This vaccine primes the immune system to recognize and fight the virus, offering significant protection if exposure occurs.
The more common scenario is post-exposure prophylaxis (PEP), which is critical after any potential rabies exposure. PEP involves thorough and immediate washing of the wound with soap and water, which helps physically remove some of the virus, followed by a course of rabies vaccine and, in some cases, rabies immunoglobulin. If administered promptly and correctly before symptoms begin, PEP is virtually 100% effective at preventing rabies. This makes public awareness and rapid medical response crucial whenever a person is bitten by an animal, particularly in regions where rabies is known to circulate.
Global efforts to eliminate rabies have made progress, yet the virus remains a substantial problem in parts of Asia, Africa, and South America. Each year, rabies kills tens of thousands of people, with the vast majority of cases occurring in children under the age of 15 who are bitten by rabid dogs. The disease is often underreported, and limited access to vaccines and medical care remains a barrier in many endemic regions. The World Health Organization, in partnership with animal health and humanitarian organizations, has set a global target to eliminate dog-mediated human rabies by 2030, highlighting the need for continued investment, vaccination campaigns, and public education.
Apart from direct vaccination and prompt PEP, public health strategies also emphasize controlling stray dog populations, improving surveillance systems, and educating communities about the risks and first aid steps after animal bites. In some cases, advanced laboratory diagnostics are used to identify the presence of rabies virus in animals and humans, helping inform public health responses and outbreak containment.
In summary, the rabies virus stands out as a medical emergency due to its almost 100% fatality rate once symptoms appear. Its ability to silently invade the central nervous system and cause irreversible brain damage highlights the importance of early intervention and robust prevention measures. Vaccination—both in animals and people—is the cornerstone of global rabies control, while rapid post-exposure care is the difference between life and death for those exposed. Public education about rabies risks, wound care, and the urgent need for medical attention after animal bites cannot be overstated. With coordinated global efforts, improved access to vaccines, and heightened public awareness, it is possible to envision a world where this ancient and terrifying disease is finally relegated to history.