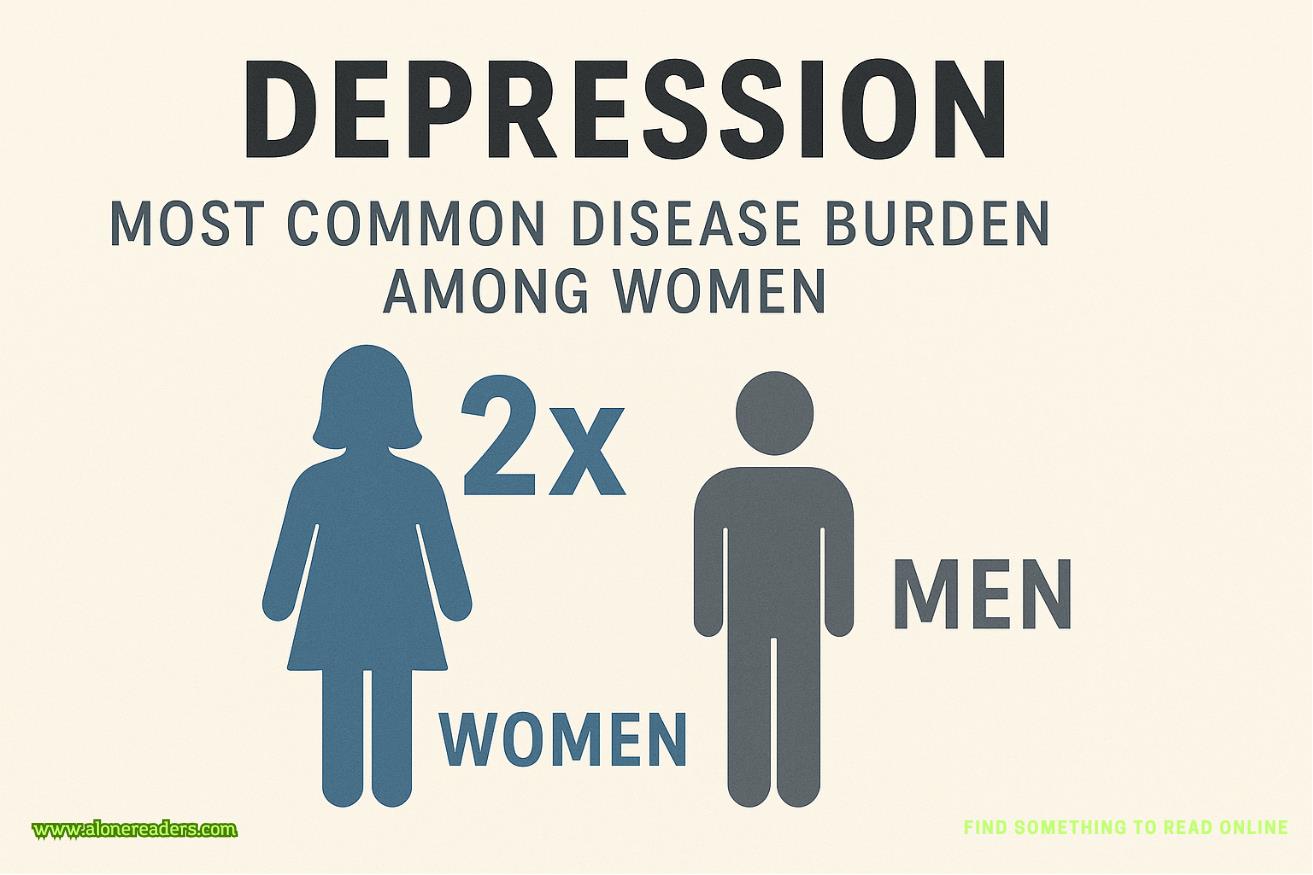
Depression is a complex mental health condition that affects millions of people worldwide, but research consistently shows that it impacts women at nearly twice the rate of men. This difference is not simply a statistical curiosity; it reflects a combination of biological, psychological, and social factors that contribute to women’s higher vulnerability. Depression in women often occurs during periods of hormonal change such as adolescence, pregnancy, postpartum, and menopause, but it is also strongly influenced by life experiences, societal roles, and cultural expectations. The World Health Organization has identified depression as one of the leading causes of disease burden among women, highlighting the urgent need for awareness, prevention, and tailored treatment strategies.
One significant contributor to this gender disparity is hormonal fluctuation. Estrogen and progesterone levels, which shift throughout the menstrual cycle and across different life stages, can influence mood regulation and stress responses. Conditions like premenstrual dysphoric disorder (PMDD) and postpartum depression illustrate how hormonal changes can trigger depressive episodes. However, hormones are not the sole explanation; many women experience depression outside of these specific hormonal phases, indicating a deeper interplay between biology and environment.
Social and cultural pressures also play a powerful role. Women are often expected to balance multiple responsibilities—career, childcare, household management, and emotional caregiving for family members—which can create chronic stress and feelings of being overwhelmed. Societal norms in many cultures discourage open discussion of mental health struggles, leading women to internalize their distress rather than seek help early. In some regions, economic dependence, lack of education, and limited healthcare access further compound these challenges, increasing the risk of untreated depression.
Trauma is another critical factor. Women are statistically more likely to experience sexual abuse, intimate partner violence, and other forms of interpersonal trauma, all of which are strong risk factors for depression. Even when the traumatic events occur in childhood, the long-term psychological impact can resurface later in life, especially during stressful periods. The combination of trauma history and ongoing stressors can make recovery more difficult without targeted therapy and support.
From a psychological perspective, women are more likely to engage in ruminative thinking—repeatedly focusing on the causes and consequences of their distress—which can prolong and intensify depressive episodes. Men, by contrast, may be more likely to use distraction or externalizing behaviors such as substance use, which can temporarily mask depressive symptoms. This difference in coping styles can partly explain why depression is diagnosed more often in women, as their symptoms may be more readily visible and reported in clinical settings.
The consequences of depression for women are profound. Beyond emotional suffering, depression can interfere with work performance, parenting, and relationships, creating a ripple effect that impacts families and communities. Physical health is also affected; women with depression are at higher risk for cardiovascular disease, chronic pain conditions, and weakened immune function. When left untreated, depression increases the risk of suicidal thoughts and behaviors, making timely intervention crucial.
Treatment for depression in women requires a multifaceted approach. Psychotherapy, particularly cognitive behavioral therapy (CBT) and interpersonal therapy (IPT), has strong evidence for effectiveness. Antidepressant medications can be beneficial, especially when combined with therapy, but healthcare providers must consider factors such as pregnancy, breastfeeding, and potential side effects. Support groups, peer counseling, and community mental health programs provide additional layers of assistance, reducing isolation and stigma.
Preventive strategies are equally important. Public health initiatives that address gender-based violence, improve access to education, and provide economic opportunities for women can indirectly reduce depression rates. Encouraging open conversations about mental health in families, workplaces, and schools helps break the cycle of silence and shame. Lifestyle interventions—regular exercise, balanced nutrition, sufficient sleep, and mindfulness practices—also contribute to resilience, though they should complement, not replace, professional treatment for moderate to severe depression.
Global health organizations emphasize that tackling depression among women is not only a mental health priority but also a broader social and economic necessity. When women’s mental health improves, entire communities benefit from increased productivity, stronger family stability, and reduced healthcare costs. This underscores the need for governments, healthcare providers, and communities to work together in building supportive environments where women can access early diagnosis, appropriate treatment, and long-term recovery resources.
In summary, depression’s higher prevalence among women reflects a complex interaction of biological vulnerability, social pressures, and life experiences. Addressing this public health challenge requires more than just medical intervention; it calls for systemic changes in how societies value and support women’s mental well-being. By recognizing the unique risks women face and ensuring they have access to effective care, it is possible to reduce the burden of depression and promote healthier, more empowered lives for women worldwide.